What has research taught us?
We are pleased to share insights into research studies on Paget's disease, providing valuable information that can significantly impact the understanding and management of this condition for patients.

Disease mechanisms and models
What goes wrong inside bone cells? Investigating the mechanisms and models of Paget's disease enhances our comprehension of the disorder, opening avenues for groundbreaking therapeutic interventions
Read more
Paget's genetics
A new gene associated with the disease revealed and molecular testing funded by the Association could enable earlier diagnosis of rare cancer
Read more
Epidemiology and patient experience
This section includes research funded by the Association into: the incidence of Paget's in the UK; Vitamin D; side effects of bisphosphonate infusions; clinical presentation; and intensive versus symptomatic treatment
Read more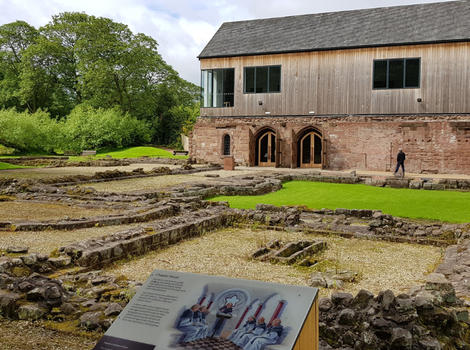
Ancient Paget’s disease
Research funding by The Paget's Association enabled scientists to unravel an 800-year-old mystery associated with Paget's disease. Photo - Norton Priory
Read more